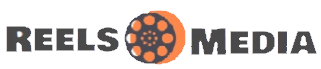
Gastroshiza, also known as gastroschisis, is a rare congenital abdominal wall defect that affects newborns. In this condition, a baby’s intestines develop outside the body through a small opening near the belly button. Although it can sound alarming, early prenatal diagnosis, timely surgical repair, and specialized neonatal care have greatly improved outcomes.
Understanding the causes, symptoms, risk factors, and treatment options is important for parents and caregivers. This guide provides a complete overview of gastroshiza, including how it is diagnosed before birth, surgical procedures, recovery, long-term outlook, and support for families, helping you navigate this condition with confidence and clarity.
What Is Gastroshiza?
Gastroshiza, also commonly known as gastroschisis, is a rare congenital abdominal wall defect that develops during early pregnancy. In this condition, a baby is born with a small opening in the abdominal wall, usually located near the belly button, through which the intestines extend outside the body without a protective sac. Because the bowel is exposed to amniotic fluid, it can become irritated or swollen before birth.
Gastroshiza is typically identified in newborns and requires immediate medical attention after delivery. Although it may sound alarming, advances in neonatal surgery and treatment for gastroshiza have significantly improved outcomes. With proper diagnosis, surgical repair, and postnatal care, many babies recover well and go on to live healthy lives.
Gastroshiza versus Gastroschisis Are They the Same?
Yes, gastroshiza and gastroschisis refer to the same medical condition in most cases. Gastroschisis is the medically accepted term used by doctors and health organizations, while gastroshiza is a common alternative spelling often used in online searches. Search engines, including Google, treat both terms as closely related and part of the same topic.
Both describe a congenital abdominal wall defect where a baby’s intestines develop outside the body through an opening near the belly button. There is no difference in symptoms, diagnosis, or treatment between the two terms. For SEO and clarity, it’s important to include both gastroshiza and gastroschisis in content so readers and search engines clearly understand the topic.
How Common Is Gastroshiza?
Gastroshiza (gastroschisis) is considered a rare birth defect, but its occurrence has increased slightly over the past few decades. It affects approximately 1 in every 2,000 to 4,000 newborns worldwide, making it uncommon but not extremely rare. Medical studies show that gastroshiza is more frequently seen in younger mothers, particularly those under the age of 20.
The condition appears across all regions and backgrounds, and it is not linked to race or family history in most cases. Because of improved prenatal ultrasound diagnosis, gastroshiza is now detected earlier during pregnancy, which helps doctors plan timely treatment. Early detection and modern neonatal care have greatly improved survival rates and long-term outcomes for babies born with this condition.
Causes of Gastroshiza
Gastroshiza, also known as gastroschisis, occurs when a baby’s abdominal wall does not fully close during early pregnancy, leaving a small opening near the belly button. Through this opening, the intestines and sometimes other organs may protrude outside the body.
The exact cause of gastroshiza is not fully understood, but several factors may increase the risk. Young maternal age, exposure to certain medications, smoking, or poor nutrition during pregnancy can contribute. It is important to note that gastroshiza is usually not inherited and is rarely linked to family genetics.
Early prenatal care, proper nutrition, and avoiding harmful substances can help reduce risks. Detecting gastroshiza early allows doctors to plan effective treatment and surgical repair, improving outcomes for newborns.
Risk Factors During Pregnancy
Certain risk factors can increase the likelihood of a baby being born with gastroshiza (gastroschisis). The condition is most commonly seen in young mothers under 20 years old, and studies suggest that maternal smoking or exposure to alcohol and certain medications during early pregnancy may raise the risk.
Other contributing factors include poor prenatal nutrition, obesity, and environmental exposures, though these links are less consistent. Importantly, gastroshiza is rarely genetic, so having a previous child with the condition does not guarantee recurrence.
Understanding these risk factors helps expectant mothers take preventive steps and ensures early prenatal screening, allowing doctors to prepare for timely diagnosis, treatment, and surgical repair after birth.
Is Gastroshiza Genetic or Inherited?
Most cases of gastroshiza (gastroschisis) are not genetic or inherited. Unlike some congenital conditions, gastroshiza usually occurs sporadically, meaning it arises randomly during early fetal development when the abdominal wall fails to close properly.
While researchers have explored potential genetic links, there is currently no strong evidence that family history directly causes gastroshiza. Instead, factors like young maternal age, lifestyle choices, and environmental exposures play a bigger role.
It’s important for parents to know that having one child with gastroshiza does not significantly increase the chance of it happening in future pregnancies. Early prenatal care, proper nutrition, and avoiding harmful substances remain the best ways to support a healthy pregnancy.
Signs and Symptoms of Gastroshiza
Gastroshiza (gastroschisis) is usually evident at birth, as the baby’s intestines protrude through a small opening in the abdominal wall near the belly button. Unlike some other abdominal wall defects, there is no protective sac, so the exposed organs are directly in contact with amniotic fluid before birth.
Newborns with gastroshiza may have swollen or irritated intestines, which can appear red or inflamed. The condition is typically pain-free at birth, but immediate medical attention is required to prevent infection and complications.
Recognizing these key signs and symptoms early allows doctors to provide prompt surgical treatment. Early diagnosis, sometimes even during prenatal ultrasounds, ensures the baby receives the best possible care and improves long-term outcomes.
Prenatal Diagnosis of Gastroshiza
Gastroshiza (gastroschisis) can often be detected before birth through routine prenatal screenings. Ultrasound examinations, usually performed around 18–20 weeks of pregnancy, can reveal the abdominal wall defect and the intestines protruding outside the fetus’s body.
Early prenatal diagnosis is important because it allows doctors to plan delivery in a specialized medical center where neonatal care and surgical repair are immediately available. In some cases, additional imaging tests may be used to assess the size of the defect and the condition of the exposed organs.
Detecting gastroshiza early gives parents time to prepare emotionally and practically, and it helps ensure that treatment and neonatal care can begin promptly after birth, improving outcomes for the baby.
What Happens at Birth? (Immediate Medical Care)
When a baby with gastroshiza (gastroschisis) is born, immediate medical attention is crucial. The exposed intestines are vulnerable to infection and damage, so doctors carefully cover them with sterile materials to protect them from harm.
The newborn is typically transferred to a neonatal intensive care unit (NICU), where doctors monitor vital signs, hydration, and body temperature. Intravenous fluids and antibiotics may be administered to prevent complications.
Prompt stabilization allows surgeons to plan the most appropriate surgical repair, whether a primary closure or a staged repair using a silo. Early intervention ensures the best outcomes and reduces the risk of long-term digestive problems or other complications.
Treatment Options for Gastroshiza
The treatment of gastroshiza (gastroschisis) is primarily surgical. The main goal is to safely place the exposed intestines back into the abdominal cavity and close the opening in the abdominal wall.
There are two common approaches: primary closure, where the intestines are returned and the opening closed in a single surgery, and staged repair using a silo, which gradually returns the intestines over several days before closing the abdomen.
Post-surgery, babies often require specialized neonatal care, including intravenous fluids, nutrition support, and monitoring for complications. With timely surgical repair and proper postnatal care, most infants recover well, and long-term outcomes are generally positive.
Possible Complications of Gastroshiza
Although gastroshiza (gastroschisis) can be successfully treated, there are potential complications that doctors monitor closely. Immediately after birth, exposed intestines are at risk for infection, swelling, and irritation.
Post-surgery, some babies may experience feeding difficulties, delayed bowel function, or, in rare cases, short bowel syndrome if part of the intestine is damaged. Other possible issues include hernia formation at the surgical site or intestinal blockages that may require further intervention.
Early detection, prompt surgical repair, and attentive neonatal care significantly reduce the risk of complications. Parents are advised to follow up regularly with their pediatric and surgical teams to ensure healthy growth, digestion, and development.
Recovery After Gastroshiza Surgery
Recovery after gastroshiza (gastroschisis) surgery is a gradual process that requires careful monitoring. Most babies spend several weeks in the neonatal intensive care unit (NICU) until their intestines function properly and they can tolerate feeding.
Initially, babies may receive intravenous fluids and nutrition, gradually transitioning to tube feeding and then to oral feeding as the digestive system recovers. Parents are taught how to care for their baby at home, including monitoring for signs of infection or complications.
With attentive postnatal care and regular follow-ups, many infants make a full recovery, achieving normal growth and development. Early medical intervention and supportive care significantly improve long-term outcomes for children born with gastroshiza.
Long-Term Outlook and Prognosis
The long-term outlook for babies with gastroshiza (gastroschisis) is generally positive, especially with early diagnosis, surgical repair, and proper postnatal care. Most infants go on to lead healthy lives, although some may experience temporary digestive issues as their intestines adapt.
Survival rates have improved dramatically thanks to advances in neonatal surgery and intensive care, with most babies achieving normal growth and development. Regular follow-ups are important to monitor digestive function, growth, and overall health.
While complications can occur, proactive medical care and parental support help children overcome challenges. With proper management, the prognosis of gastroshiza is encouraging, giving parents hope for a healthy future for their child.
Life Expectancy and Quality of Life
Babies born with gastroshiza (gastroschisis) generally have a normal life expectancy when the condition is diagnosed early and treated promptly. Advances in neonatal surgery, NICU care, and postnatal monitoring have significantly improved survival rates.
After recovery, most children experience healthy growth and development, attend school, and engage in normal physical activities. Some may have minor digestive issues early on, but these typically resolve with time and proper care.
Quality of life is further enhanced by ongoing medical follow-ups, nutrition guidance, and parental support. With attentive care and early intervention, children with gastroshiza can thrive and enjoy a full, active life similar to their peers.
When to Seek Medical Advice
Parents of babies with gastroshiza (gastroschisis) should stay vigilant even after successful surgery. It is important to seek immediate medical attention if the baby shows signs of infection, such as redness, swelling, fever, or unusual discharge at the surgical site.
Other warning signs include persistent vomiting, feeding difficulties, abdominal swelling, or changes in bowel movements. Regular follow-up visits with pediatric surgeons and neonatologists are crucial to monitor growth, digestion, and overall health.
Prompt medical evaluation helps prevent complications and ensures the baby continues to recover well. Early intervention, combined with attentive home care and medical guidance, supports the long-term health and well-being of infants with gastroshiza.
Final Thoughts
Gastroshiza, also known as gastroschisis, is a rare but manageable congenital abdominal wall defect. Early prenatal diagnosis, prompt surgical repair, and attentive neonatal care are essential for achieving the best outcomes. While the condition can be alarming for parents, medical advances have greatly improved survival rates, recovery, and long-term health.
Understanding the causes, risk factors, symptoms, and treatment options helps parents and caregivers make informed decisions and prepare for the newborn’s care. With proper support, guidance, and follow-up, most children with gastroshiza go on to lead healthy, normal lives. Awareness and education remain key to navigating this condition with confidence and hope.
FAQs
Is gastroshiza life-threatening?
With early diagnosis, prompt surgical repair, and proper neonatal care, gastroshiza (gastroschisis) is rarely life-threatening. Most babies recover fully and lead healthy lives.
Can gastroshiza be prevented?
There is no guaranteed way to prevent gastroshiza, but early prenatal care, proper nutrition, and avoiding smoking or harmful substances during pregnancy can reduce risk factors.
Does gastroshiza affect future pregnancies?
Gastroshiza is usually not inherited, so having one child with the condition does not significantly increase the risk in future pregnancies.
How is gastroshiza treated?
Treatment involves surgical repair, either a single-step closure or staged repair using a silo, combined with NICU care and postnatal support.
What is the long-term outlook?
Most children experience normal growth and development. Some may have minor digestive issues initially, but long-term outcomes are generally positive.